Robotic Process Automation (RPA) has been adopted by health systems across the country. The ability to automate repetitive tasks in the revenue cycle offers health systems and hospitals an opportunity to gain efficiencies (speed) in their processes. While RPA is a powerful tool in the revenue cycle, it has limitations:
- Bots Break - RPA bots are programmed. A series of steps are built and the bot follows the rules. This automates action, but is a rigid system. Every time a step changes, the bot breaks. In healthcare payments, bot are up against ongoing changes. Insurance payers are constantly changing the processes, and even little changes, like field location or spacing edits count as step changes and can derail RPA. CIO reports that breaking bots is the number one reason RPA projects fail (the RPA Death Spiral).
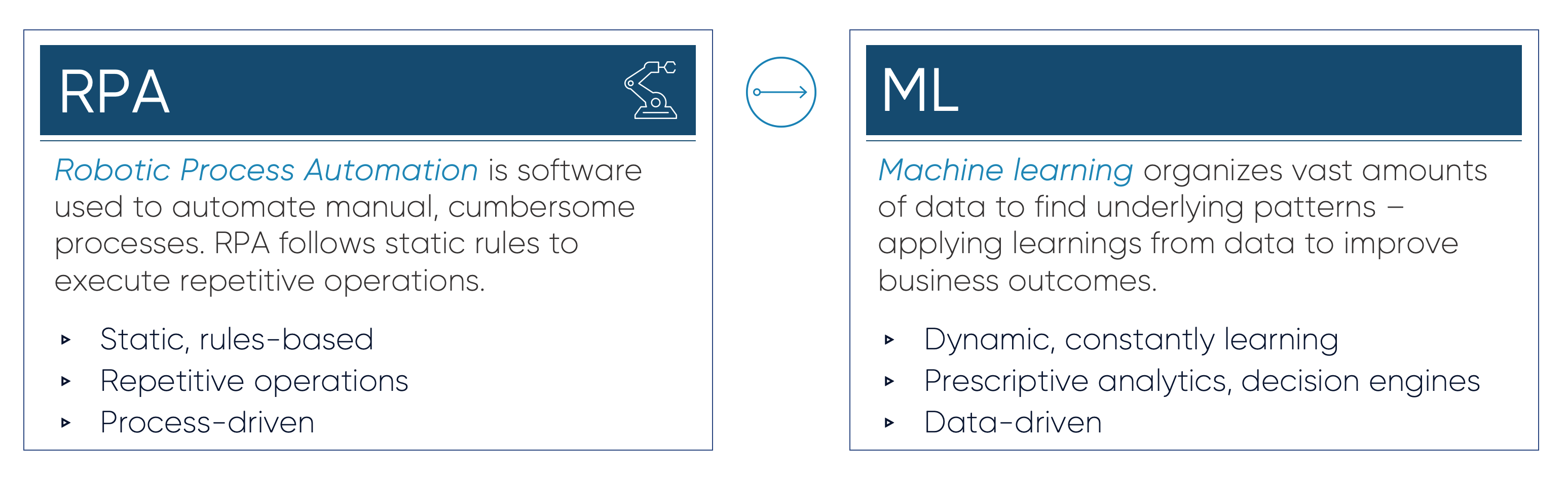
- Bots are Simple - “Robotic Process Automation” sounds advanced and intelligent, but it’s simply a set of programmed rules -- it should not be mistaken for AI. RPA doesn’t learn and requires ongoing oversight by humans. While RPA offers efficiencies, saving time on repetitive tasks, RPA doesn’t provide any sort of dynamic intelligence.
- Bots Require Expensive Humans - RPA requires consultants — consultants program and update the bots and are needed on an ongoing basis. For every $1 spent on RPA an additional $3.41 is spent on consulting resources. (Forrester Research, 2019)
When humming along, RPA automates tasks to gain efficiencies. But, efficiency and intelligence are different. Health systems have to move beyond automation to truly improve payment outcomes. In healthcare payments, machine learning can complement RPA, adding decision intelligence to revenue cycle workflows, and offer a different route to optimize processes and strategy. The revenue cycle needs intelligence — this means going beyond RPA.
Machine learning enables health systems to *learn* from their payments data — and without the ongoing programming required by RPA. Machine learning organizes mountains of healthcare payments data and detects underlying patterns. These underlying patterns are used to predict future behavior and to prescribe the strategies that drive the most optimal payment outcomes.
RPA can make revenue cycle processes faster and help eliminate human errors -- machine learning goes beyond automation, unlocking true insights and root cause analysis that allows for the prioritization of the next best action in the revenue cycle. It’s the difference between working faster and working smarter.
RPA is Fast. Machine Learning is Smart (and Fast).
Sift’s machine learning provides standalone intelligence and strategic insights, or compliments RPA tools with data-driven inputs. Learn more about Sift’s machine learning solutions for healthcare payments.






